An arrhythmia is an abnormal sinus rhythm with normal atrioventricular (AV) conduction.
Normal sinus rhythm originates from the sinus node in the upper portion of the right atrium. During sinus rhythm, the heart rate is in the normal range, the P waves are normal on the electrocardiogram (ECG), and the rate is stable.
The normal sinus rate at rest is considered to be between 60 and 100 beats per minute (bpm). However, the range (defined by two standard deviations from the mean) is between 43 and 93 bpm for men and 52 and 94 bpm for women. Sinus bradycardia or tachycardia may be physiologic (i.e., normal) or non-physiologic (i.e., abnormal).
Not uncommonly, the activation rate of the sinus node varies, leading to a variable P-P interval on the ECG. If the variation of the P-P interval is 0.12 sec (120 ms) or more in the presence of normal P waves, it is known as sinus arrhythmia. Sinus arrhythmia is usually physiologic and is related to respiratory cycles. It does not require treatment.
Classification
Cardiac arrhythmia can be classified in various ways.
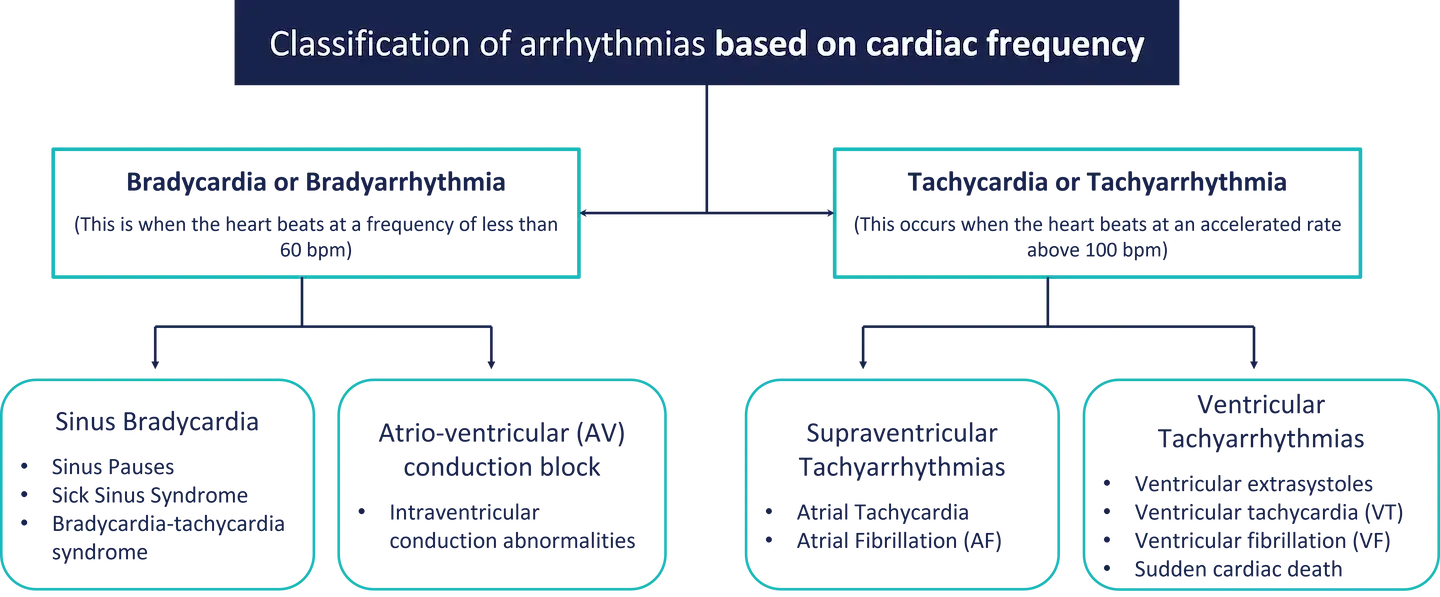
1. Based on the cardiac frequency
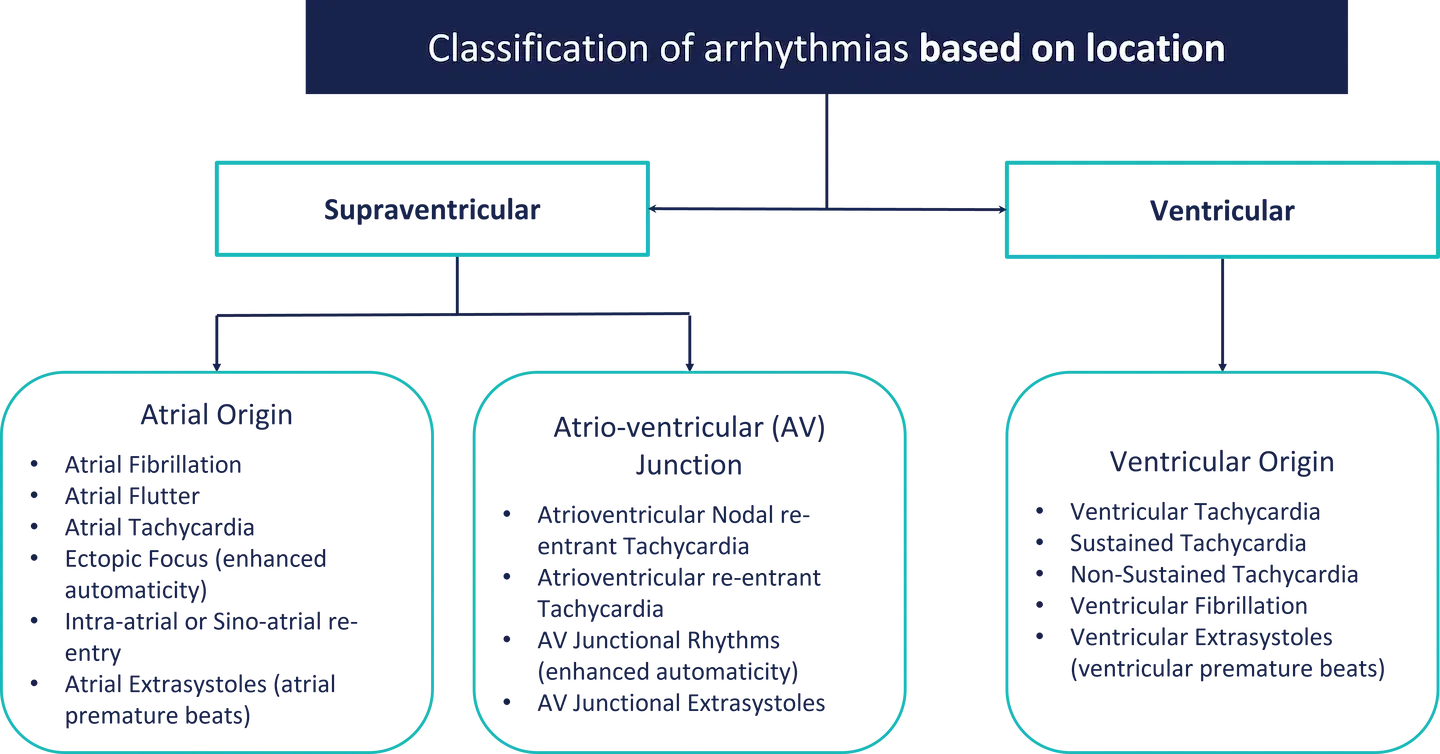
2. Based on location
Cardiac arrhythmias can be of different types depending on the area of initiation in the heart.
Symptoms and signs of arrhythmia
Patients with cardiac arrhythmias exhibit a wide spectrum of clinical presentations, ranging from asymptomatic incidental ECG abnormalities to survival from sudden cardiac arrest (SCA). Their history is key to directing the evaluation of patients. A family history of a significant cardiac arrhythmia may not directly inform the prognosis of a patient.
1. Palpitations
Palpitations are signs of awareness of the heartbeat, and they may be caused by a rapid heart rate, irregularities in heart rhythm, or an increase in the force of cardiac contraction. Patients who complain of palpitations describe the sensation of unpleasant awareness of a forceful, irregular, or rapid beating of the heart.
2. Syncope, Presyncope, and Altered Level of Consciousness
Syncope, commonly referred to as “fainting” or “passing out,” is a transient, self-limited loss of consciousness and posture resulting from a drop in blood pressure with cerebral hypoperfusion. It is important to distinguish syncope from other causes of transient loss of consciousness, such as seizures, metabolic disorders (hypoglycaemia), hypoxia, intoxication, cataplexy, and pseudo syncope. When syncope is caused by a cardiac arrhythmia, its onset is rapid and the duration is usually brief, with or without a preceding aura, and it is not typically followed by a postictal confusion state.
Common arrhythmic causes of syncope include bradyarrhythmia caused by sinus node dysfunction or AV block and tachyarrhythmias, most often ventricular, but on occasion supraventricular. Bradycardia can follow tachycardia in patients with the bradycardia-tachycardia syndrome.
· Sudden Cardiac Arrest and Sudden Cardiac Death: SCD caused by cardiac arrhythmias is most often the result of VT or ventricular fibrillation (VF). However, it can result from profound bradycardia, as might be observed in complete heart block or asystole.
REFERENCES
1. Giada F, Raviele A. Clinical approach to patients with palpitations. Card Electrophysiol Clin. 2018;10:387–396.
2. Goldberger ZD, Petek BJ, Brignole M, et al. ACC/AHA/HRS versus ESC guidelines for the diagnosis and management of syncope: JACC guideline comparison. J Am Coll Cardiol. 2019;74:2410–2423.
3. Puppala VK, Akkaya M, Dickinson O, et al. Risk stratification of patients presenting with transient loss of consciousness. Cardiol Clin. 2015;33:387–396
4. Kim J, Kwon M, Chang J, et al. Meta- analysis of prognostic implications of exercise- induced ventricular premature complexes in the general population. Am J Cardiol. 2016;118:725–732.
5. Skinner JR, Winbo A, Abrams D, et al. Channelopathies that lead to sudden cardiac death: clinical and genetic aspects. Heart Lung Circ. 2019;28:22–30.